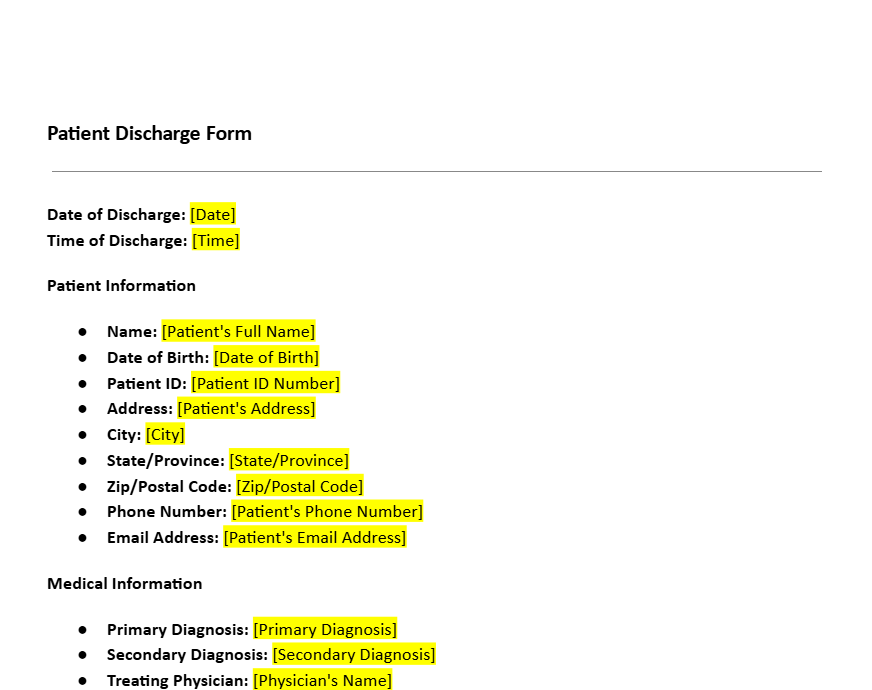
Patient Discharge Form Template
8 Downloads
Healthcare & Social Services Agreements
March 4, 2025
FreshDox
Patient Discharge Form Template: Create Clear, Safe & Compliant Hospital Discharge Summaries
A patient is never more vulnerable than in the hours and days after leaving the hospital. A clear, well-structured patient discharge form is often the difference between a smooth recovery at home and an avoidable readmission. That is why hospitals, clinics, and healthcare providers around the world rely on a standardised hospital discharge form template to capture everything the patient and care team need to know when inpatient care ends.
A medical discharge form documents the patient’s condition, treatment, and aftercare plan at the time of discharge. It keeps healthcare practitioners aligned on what has been done, what comes next, and what the patient must watch for after leaving the facility. It also gives patients and caregivers a written roadmap to follow once verbal instructions are forgotten.
Using a structured patient discharge form template improves communication between physicians, nurses, allied health professionals, and follow-up care providers. It also reduces post-discharge complications, enhances the patient experience, and supports medico-legal compliance. Below, we explore why discharge documentation matters, what to include in your hospital discharge summary form, and how a ready-to-use template from FreshDox can streamline your workflow.
Why Hospitals and Healthcare Providers Need a Patient Discharge Form
1. Consent and Permission at the Point of Discharge
Before leaving the hospital or clinic, patients are typically asked to sign a patient discharge form acknowledging that they understand the doctor’s instructions and the recommended aftercare plan. Their signature confirms that:
- They have received discharge instructions in a language and format they understand.
- They accept the recommended plan for home care or follow-up treatment.
- They know whom to contact if symptoms worsen or new problems appear.
In cases of discharge against medical advice (DAMA), a specific consent section or a separate DAMA acknowledgement can be integrated into the same discharge form template. This documents that the risks of leaving early were explained, and that the patient chose to leave despite those recommendations.
When ongoing treatment with another provider is required, the hospital discharge form can also record the patient’s consent to share relevant medical information with the receiving clinician, rehabilitation centre, or home-care agency.
2. Compliance with Laws, Regulations and HIPAA
Healthcare providers must meet strict privacy and documentation standards. A properly structured medical discharge form template supports compliance with:
- HIPAA or other local privacy regulations regarding handling of patient information.
- Hospital accreditation standards related to discharge planning and documentation.
- Payer and insurer requirements for demonstrating medical necessity and continuity of care.
Clear language about confidentiality, record access, and information sharing helps patients understand their rights. Documented discharge summaries and signed acknowledgment forms protect both the healthcare facility and the patient by showing that discharge education and planning were properly completed.
3. Better Form Functionality and Integration with EMR
A modern patient discharge summary form should work across both paper and digital environments:
- Editable PDF or Word formats for printing and bedside completion.
- Digital versions integrated with electronic medical records (EMR/EHR) systems for quick retrieval and audit.
- Standardised fields so physicians, nurses, and allied health staff follow the same structure on every discharge.
Using a pre-built patient discharge form template ensures consistency across departments—emergency, ICU, wards, day surgery, and outpatient clinics. It helps reduce clerical errors, speeds up discharge processing, and makes information easier to find later.
4. Seamless Integration with Hospital Workflows
Most facilities weave the hospital discharge form into their broader admission–treatment–discharge cycle. A good template can be linked to:
- Admission and registration forms for quick demographic pull-through.
- Medication charts, operative notes, and nursing records.
- Requests for home-care services, medical devices, or physiotherapy.
- Feedback sections capturing the patient’s experience of care.
Used properly, the discharge form becomes a central communication tool between hospital teams, community providers, and families, rather than just a piece of paperwork to “tick off” at the end.
Key Sections to Include in a Patient Discharge Form
1. Basic Patient Information
Every patient discharge form should begin with clear identifiers so that the document is correctly linked to the patient’s medical record. At minimum, include:
- Full legal name (as per government ID).
- Date of birth.
- Hospital ID or medical record number.
- Residential address and up-to-date contact details.
- Emergency contact person and relationship.
Accurate demographic information minimises administrative errors, supports safe follow-up, and ensures the discharge summary can be located quickly by any member of the care team.
2. Summary of Medical History and Hospital Course
The patient discharge summary form should briefly recap relevant medical history and the care provided during the stay. This usually includes:
- Key pre-existing conditions that impact current treatment.
- Allergies and documented drug reactions.
- Primary diagnosis and significant secondary diagnoses.
- Important events or complications during the admission.
For surgical or procedural cases, include the type of procedure, date performed, outcome, and any intra-operative or post-operative issues. This concise narrative helps future clinicians understand what has already been done and what to monitor going forward.
3. Reason for Hospital Admission
This section explains why the patient was admitted and provides context for the rest of the discharge summary. Typically, it includes:
- Presenting symptoms and duration.
- Working diagnosis on admission.
- Initial investigations, imaging, and lab tests requested.
- Any relevant social or functional factors (e.g., living alone, mobility issues).
Clear documentation of the admission reason makes internal audits easier and supports quality improvement, coding, and billing processes.
4. Major Medical Findings and Final Diagnosis
Based on the full hospital course, the hospital discharge form should set out the main medical findings, including:
- Final discharge diagnoses.
- Key lab results and imaging findings that influenced treatment.
- Response to therapy and status at discharge (e.g., stable, improved, palliative).
This becomes a critical reference point for future admissions, outpatient clinics, and primary care providers who will continue the patient’s long-term management.
5. Procedures and Services Provided
Every significant intervention during the stay should be listed in the medical discharge form, such as:
- Surgeries, endoscopies, and invasive procedures.
- Specialist consultations (cardiology, psychiatry, physiotherapy, etc.).
- Blood transfusions or high-risk therapies.
- Diagnostic tests with important findings.
This formal record of services supports continuity of care, provides a transparent clinical trail, and assists with billing and claims.
6. Condition at the Time of Discharge
Before leaving, the patient’s status should be summarised in simple, clear language, answering questions like:
- Is the patient clinically stable to go home or transfer?
- What symptoms are expected and what are red-flag warning signs?
- Are there mobility, self-care, or cognitive limitations?
This section also supports insurers and case managers in understanding why specific home-care services, aids, or follow-up visits are required.
7. Discharge Instructions and Follow-Up Plan
Perhaps the most critical part of the patient discharge form template is the aftercare section. This should include:
- Medication list: names, doses, timing, start/stop dates, and any discontinued medicines.
- Self-care instructions: wound care, activity restrictions, lifting limits, driving or work advice.
- Dietary recommendations: special diets, fluid restrictions, or nutritional supplements.
- Warning signs: symptoms that require urgent review or emergency attention.
- Follow-up appointments: dates, times, and locations for clinic visits or tests.
- Referrals: home-health nursing, physiotherapy, occupational therapy, counselling, or specialist clinics.
Clear, plain-language instructions—supported by a written hospital discharge form PDF the patient can take home—dramatically reduce the risk of confusion and readmission.
8. Physician’s Signature and Contact Details
The discharge is completed only once the attending physician (and where required, the nurse in charge) signs the patient discharge form. The signature confirms that:
- The clinical information recorded is accurate.
- Discharge criteria have been met.
- Education and aftercare planning have been explained to the patient or caregiver.
Including direct contact information for the ward, department, or clinic helps patients know exactly where to call if they need clarification after going home.
Download a Patient Discharge Form Template with a Free Trial of FreshDox
If you are still creating discharge summaries from scratch or copying old forms, you are spending precious clinical time on formatting instead of patient care. A professionally drafted patient discharge form template from FreshDox makes it simple to standardise your process, improve documentation quality, and stay compliant.
With FreshDox, you can:
- Access a ready-to-use hospital discharge form template in Word and PDF formats.
- Customise sections to match your internal policies, EMR fields, and speciality needs.
- Reuse the same structure across wards, clinics, and locations for consistent, high-quality documentation.
- Browse an entire library of healthcare form templates—admission forms, consent forms, progress notes, and more.
Sign up for a free 7-day trial of FreshDox to download the Patient Discharge Form Template and start streamlining your discharge workflow today. Whether you manage a hospital, day-surgery centre, or private clinic, our templates help you reduce risk, support safer aftercare, and make documentation faster and more accurate for your whole team.
Related Templates
Discover more templates that align with your needs and preferences.
Ready to Sign Up?
Start your 7-day free trial and access professionally drafted legal documents built for business use.
- Cancel any time
- 7-day free trial
- From 300+ Customer Reviews