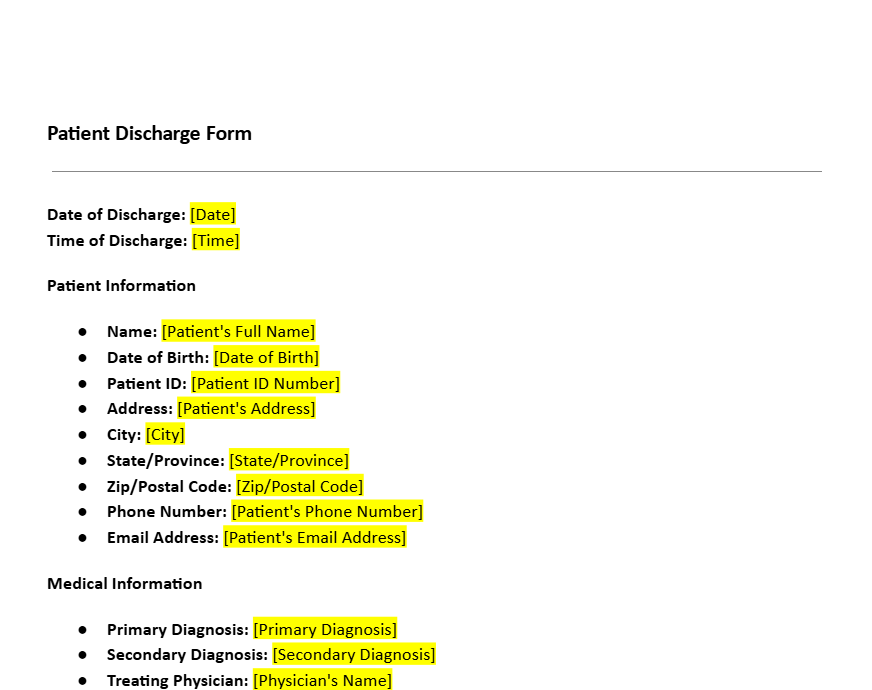
Patient Discharge Form Template
8 Downloads
Health and Social
March 4, 2025
Sayantani Dutta
A discharge form is used in healthcare facilities to outline a patient’s discharge from a healthcare facility or hospital. It not only keeps healthcare practitioners abreast of patient care but also clearly instructs patients on what to expect during the outpatient phase of their aftercare.
A formalized, comprehensive discharge summary enhances communications between healthcare providers, patients, and follow-up care providers. A comprehensive patient discharge form can also avert post-discharge complications.
Discharged patients must be vigilant regarding their awareness signs that can be a precursor to problems in their aftercare plan. The discharge form provides a formal written reference that complements verbal instructions from healthcare practitioners.
Why Hospitals and Healthcare Providers Need a Patient Discharge Form
Consent and Permission
Before being discharged from the hospital, patients sign a discharge form that affirms they have accepted and understood the doctor’s instructions. They acknowledge the aftercare protocol in the outpatient phase of their care by signing the discharge form. This documentation is a testament that the patient is cognizant of the requirements of their aftercare plan.
Consent forms can also be included in case a discharge is made against medical advice. Under these circumstances, a formal report will outline the risks involved in the patient failing to continue with their treatment. If a patient requires ongoing care from another provider, a discharge form allows the release of medical information to appropriate healthcare professionals.
Compliance with Laws and HIPAA Requirements
Healthcare practitioners are obligated to use discharge forms that meet the requirements of privacy legislation. A declaration that the healthcare provider is HIPAA compliant attests to the doctor’s awareness to treat patient information securely and preserve confidentiality.
Patients are made aware that they have a right to view their medical records and they can request a copy of their discharge form when necessary. Compliance with ethical and legal requirements improves accountability and safeguards both healthcare facilities and patients.
Form Functionality and Integration
A patient discharge form should be made available in hardcopy and digital formats. Most hospitals use a form creator to produce editable, printable copies of the discharge form so healthcare personnel can process discharges efficiently.
A pre-filled form template standardizes form fields consistently and accurately across departments. Digital forms integrate with hospital electronic medical records and patient databases for easy searching and access by healthcare teams.
Medical forms can be tied in with admission forms for efficient review by healthcare insurers regarding patient aftercare requirements. Healthcare facilities using digital patient engagement solutions integrate discharge forms to simplify data collection data tracking.
Integrating the Form with Healthcare Workflows
Most hospitals integrate discharge forms into more extensive registration forms and patient management workflows. Discharge forms from hospitals are frequently tied in with request forms for additional treatments, refilling drug prescriptions, or medical devices necessary for in-home care.
Some forms feature a follow-up service questionnaire surrounding the patient’s experience with the care they received from the doctor, and nursing staff, and their overall impression of the quality of care they received, and the condition of the facilities during their stay. A patient discharge form is a vital channel of communication between healthcare providers, patients, and caregivers.
Provisions to Include in a Patient Discharge Form
Basic Patient Information
A patient discharge form for a patient should include necessary identification information. The full legal name of the patient must be included so that the paper is appropriately linked to their medical history.
The form includes the patient’s date of birth for easy identification confirmation and to reduce administrative error. Address and contact information are also recorded in case a follow-up appointment is necessary.
Summary of Medical History
The patient discharge form summarizes the patient’s medical history and the care they’ve received for these conditions. Accurate documentation of in-patient diagnoses provides physicians and healthcare providers with an explanation of the treatment they received during their stay at the facility.
If a procedure or surgery is performed at the healthcare facility, the form mentions the type of procedure, its outcome, and the follow-up care for the patient. Details about known allergies or known contra-indications to treatments or medicines must be specified so clinicians are alerted to any possible patient risks when prescribing medicines.
Reason for Hospital Admission
This section is a full explanation of why the patient is in hospital. The section includes a brief report on presenting symptoms on arrival, as well as early diagnostic studies performed to establish the patient’s medical condition.
Medical background is also taken into account, especially in case preexisting illness affects hospitalization. Clarity is critical as it forms the foundation on which care is documented. Changes to this section can be made according to administrative audit or hospital reporting requirements.
Major Medical Findings
Based on the cause for admission, this section of the form reports on discharge diagnoses established by healthcare practitioners during the patient’s hospital stay. All pertinent information from imagery, labs, and studies that went into establishing a final diagnosis are included. The information is vital in determining a patient’s condition at discharge and reference guidelines for continuing medical care.
Procedures and Services Offered
All treatments carried out in the course of a hospital stay are accounted for in this section. Any procedure, consultation, or treatment carried out by healthcare practitioners is included. The section acts as formal documentation of care.
Condition at the Time of Discharge
This section documents the state of the patient’s health at discharge from the hospital. It mentions any ongoing care requirements after discharge which is vital for the patient when submitting claims for these expenses to their healthcare insurer.
Discharge and Follow-Up Instructions for Aftercare
Discharged patients require a clear understanding of how to take care of themselves after they leave the hospital. Discharge forms have instructions on self-care directed specifically to the patient’s condition.
These guidelines can include dietary restrictions, activity advice, and instructions about wound care where appropriate.
For surgical patients and those with chronic illness, instructions on monitoring symptoms and warning signs of post-discharge complications are necessary. Scheduled specialist or primary care physician follow-up visits are recorded on the form, with a formal plan established for ongoing care.
The form will list any patient referrals to specialist clinics, home healthcare providers, or therapists. When inpatient care is not warranted, discharge forms can be customized with recommendations for physical therapy, rehabilitation, or additional medical treatment.
Notifications on patient-critical post-discharge information, i.e., changes in medication or test outcomes, must be included. By providing structured care information in hospital release forms at discharge, medical professionals reduce the risks of recovery complications and hospital readmission.
Physician’s Signature
Discharge is finalized after the attending physician signs to patient’s discharge form. The signature attests that the information in the report is a true representation of care and that the doctor has provided discharge aftercare planning to the patient.
Download a Patient Discharge Form Template with a Free Trial of FreshDox
Sign up for a free 7-day trial of FreshDox and get immediate access to our professionally designed patient discharge form template. Browse our catalog of templates for healthcare providers and use our templates to standardize your systems. Our hospital discharge form template is fully customizable to your internal processes and available to download in PDF and Word formats for your convenience.
Related Templates
Discover more templates that align with your needs and preferences.

Ready to Sign Up?
Sign up for FreshDox.com’s 7-day trial and discover why so many individuals and businesses trust us for their legal document template needs.
- Cancel any time
- 7-day free trial
- From 300+ Customer Reviews